
Cartilage Preservation and Restoration

Cartilage Preservation and Restoration
Preserving Mobility with Advanced Cartilage Treatments
The St. Luke's cartilage preservation and restoration program is dedicated to the treatment of patients with symptomatic cartilage damage, including isolated cartilage defects, meniscal injuries and early arthritis. Our expert physicians will evaluate and recommend treatment options to match the physical demands of each patient's lifestyle.
Our philosophy is to repair the cartilage damage by treating the whole patient and determining the underlying causes of damage, which can include malalignment, ligament instability and loss of meniscal function. We'll also educate patients on the safest and latest treatment options to help them to make the most informed decision regarding their cartilage damage. Conservative, or nonsurgical, management is usually attempted before more invasive, surgical options are considered.
Our patients also have access to local and national cartilage repair and restoration research projects through partnerships with St. Luke's Applied Research and Boise State University.
For more information on our cartilage preservation and restoration program, please call (208) 706-9118.

Our goal is to help you move freely and live fully so you can get back to doing what you love at home, at work, or at play.
Non-Surgical Approaches to Cartilage Repair and Preservation

Lifestyle Changes
Avoid aggravating activities, brace your joints for comfort, or begin physical therapy to improve strength and motion.

Therapeutic Joint Injections
Used to help with pain and limited motion, corticosteroid or visco supplement injections can provide relief and improved joint function.

Physical Therapy
Our physical therapists can help you gain strength, increase range of motion, and restore mobility.

Platelet-Rich Plasma
This therapy involves injecting your own platelet-rich plasma into an arthritic joint or injured tendon.
Surgical Approaches to Cartilage Repair and Preservation

Osteochondral Autograft Transplantation (OATS)
Repairs damaged cartilage by harvesting and transplanting healthy cartilage from a non-weight bearing joint area.

Matrix-Associated Autologous Chondrocyte Implantation (MACI)
Biopsies of your healthy cartilage are used to grow additional cartilage in the lab for implantation.
Microfracture
This technique makes small holes in the bone below the cartilage defect to increase blood supply and promote healing.

Osteochondral Allograft (OCA)
Donor bone and/or cartilage may be used to repair cartilage defects, with a low risk of reaction to the donor tissue.

Patellofemoral Arthroplasty
Artificial joint resurfacing to treat patients with bone-on-bone osteoarthritis in the patellofemoral compartment of your knee.
Meniscal Transplantation
Typically appropriate for younger, active patients, this offers significant pain relief and improved function.

Hip Cartilage Repair
Removes unstable cartilage, while microfracture helps restore the joint with scar tissue that behaves like cartilage.

Foot and Ankle Cartilage Repair
Techniques include microfracture or drilling of the lesion, grafting cartilage and bone, or fixation of fragments with screws.
Your Treatment Plan and Recovery
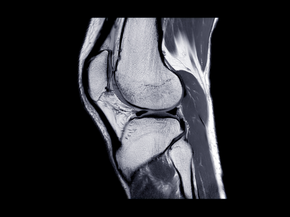
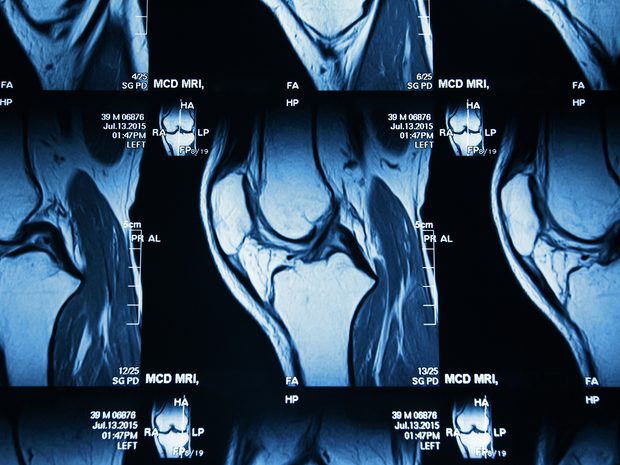
First, your surgeon will obtain x-rays to evaluate your joint and determine whether or not you're a candidate for cartilage restoration surgery. Advanced imaging, such as an MRI, is usually necessary to assess cartilage defects and develop a treatment plan.
If your treatment plan involves surgery, you should know that most cartilage restoration surgeries are outpatient procedures, which means you'll go home after your procedure rather than stay in the hospital overnight. The majority of patients will begin slowly bending and straightening the joint soon after surgery to promote healing and improve motion.
Physical therapy typically begins a couple of weeks after surgery. You may be asked to wear a brace for the first 4-6 weeks after surgery; full recovery takes approximately 6-8 months for high-intensity sports or activities.

